In this interview, virologist Prof. Bodo Plachter walks us through the race for a vaccine and a treatment against the coronavirus.

University of Mainz
Bodo Plachter has been a Professor at the University of Mainz since 1996. He’s the deputy director of the Institute for Virology at the University Medical Center Mainz and is known from countless radio and television interviews. One of his research interest focusses on the development of a vaccine against human cytomegalovirus.
Virologists are experts in high demand right now. But what do virologists actually do?
They may have different functions. One field of activity relates to patient care in a hospital. This encompasses work to oversee diagnostic testing and to guide the prevention of infections, to perform studies and, increasingly, also to visit hospital wards to counsel clinicians that encounter problems in order to help patients. Another function is to perform fundamental research. Basic researchers deal with very complex problems, do a detective’s groundwork in order to better understand viral infections and find ways how to prevent and treat them. This line of work is very close to that of a molecular biologist. Then, of course, there is also another branch that deals with questions of how viral infections spread across the population, and which mutations appear. These are called epidemiologists.
You’ve been in virology for more than 35 years. How has technology changed the field?
The biggest change has been brought about by IT resources that have allowed us to gather and analyze very large data sets. This has given rise to a lot of new insights and fields of research such as all kinds of -omics, for example, proteomics, interactomics and so on.
Which means?
Viruses need cells to multiply. What we can do, for instance, is to compare infected to uninfected cells and look at the expression levels of different proteins. An increase or decrease may be related to viral infection and thus may provide clues on how the virus interacts with its host. The large-scale study of all the proteins in cells which is enabled by information technology and genetics is called proteomics, and it has advanced the field of virology decisively. Based on such insights, hypotheses can be formulated and experiments can be carried out in the lab to test them. In the case of SARS-CoV-2, there is a huge amount of data that has been collected, including data about genetic mutations that are relevant in the context of the search for a vaccine.
What is the difference between a vaccine and a therapeutic?
A vaccine is prophylactic and used to prevent infections while a therapeutic is used when a patient is already infected and presents himself with specific symptoms. If you look at infections that are caused by bacteria, – we have powerful medications available that directly attack the bacterial cells – commonly known as antibiotics. In the case of viruses, however, there are medications available against a limited number of viruses only and often they don’t work that well, as in the case of influenza. The reason why it is so hard to come up with a therapeutic is that the viruses occupy the human cells and make use of cellular proteins for their own purpose. Targeting these processes with drugs concomitantly targets the cell and may lead to severe adverse effects. Still, some viruses induce virus-specific enzymes which may be attacked with limited adverse effects. The antiviral drug Remdesivir, which is touted as a possible treatment of Covid-19, attacks an enzyme that enables the multiplication of viral RNA. But I’m not convinced that this approach will be the breakthrough people are looking for. A completely different and well-known approach is the use of antibodies. Some antiviral antibodies are suitable to neutralize a virus because they can identify it, bind to it and thus prevent infection of the cell.
“There would be a very high acceptance by clinicians to use antibodies as therapy.”
Does that mean that in the category of therapeutics, antibodies are a safer bet than antivirals?
At the moment we have no useful antiviral therapeutic against Covid-19. I’d say there would be a very high acceptance by clinicians to use antibodies as therapy. This is because it is a strategy they already know and they are experienced with it the treatment of other diseases. Antibodies are widely used against tumors already, rituximab is an example of a blockbuster drug against cancer. The goal would be to have an antibody available for Covid-19 treatment that would help preventing severe manifestations, such that lead to artificial ventilation and intensive-care treatment. This, in consequence would help alleviate the pressure on the healthcare system. In contrast to that, I think it is questionable if we ever get efficient antivirals against Sars-CoV-2. There is a long-standing research effort to identify an efficient antiviral drug against respiratory syncytial viruses (RSV) mediated disease without significant success. Pharmacological development takes 5 to 10 years and it is a process of trial and error. Most of the studies with antiviral medications fail. Considering this, the most likely avenue for a therapeutic regimen may have to focus on a combination, e.g. of Remdesivir with a therapeutic antibody. A combination of medications like in the case of HIV reduces the risk of viruses developing resistance.
Let’s talk a bit more about the quest for a therapy based on antibodies. Apparently, some people are better at producing virus-neutralizing antibodies than others. Why?
This concept of the “super neutralizing antibodies” as they are called has really only been developed and examined in the past few years, thanks to modern technology. Indeed, in the course of a viral infection, the immune system will produce many different antibodies that target different kinds of proteins of the virus. Many of these antibodies don’t neutralize the virus at all, and we don’t know why. Some of them, however, which are developed just by a few patients, are very specific to the virus and are able to neutralize it at very low concentrations. Here again, it is unclear why exactly these individuals produce super neutralizing antibodies. But we have technologies available now to identify them. And, what is more important, we can analyze the specific B cell that produces these powerful antibodies. We can clone the cell and characterize it genetically in order to replicate this information and feed it into a production process for a therapeutic antibody. This is the charm of the whole story. And this approach has attracted a lot of interest in different applications, be it HIV, the cytomegalovirus or the BK virus.
Why do genetic mutations of a virus pose as a problem in the case of a therapeutic or vaccination?
With vaccination, you may encounter the problem that, at some point, it might lose its efficacy due to mutation. Then you need to adapt the vaccine. The best example is the influenza vaccine which needs to be adapted to target mutated viral strains almost every year. A vaccine primes our adaptive immune system against a specific pathogen. Amongst other immunologic mechanisms, that leads to the production of a wide array of antibodies. But if you want identify a therapeutic antibody, you may take care to look for one that binds to a part of the virus that does not mutate. Many viral proteins can and do mutate, but some regions are conserved. In the case of the coronavirus, some parts the spike proteins, the protein you see on all these pictures as a “Corona”, are highly conserved. This is because the virus needs these portions of the spike protein for its infection. If one is successful in identifying a neutralizing antibody that binds to these sections of the spike protein, then chances are high that this antibody is broadly effective against the different variants of SARS-CoV-2.
Will there eventually be no more need for treatment if there is a vaccine?
First of all, a vaccine needs to be found. But this may be a long way. AstraZeneca just put its phase 3 Covid vaccine trial on hold because of severe adverse events in a vaccine. Even once a vaccine is developed, many people won’t get vaccinated and it might not work in all cases. On the contrary, once a therapeutic is established and will be integrated into the standards of care, the demand will increase and prevail at a high level. But eventually, with the availability of therapeutic options and vaccines, Covid-19 will fade from public attention. Then, the economic consequences of the pandemic will take center stage.
Written by
WITH US, YOU CANCO-INVEST IN DEEP TECH STARTUPS

Verve's investor network
With annual investments of EUR 60-70 mio, we belong to the top 10% most active startup investors in Europe. We therefore get you into competitive financing rounds alongside other world-class venture capital funds.
We empower you to build your individual portfolio.
More News
29.07.2021
Why we invested
in Otoqi
Following the announcement of our 10th investment in France, we explain the reasons for our investment in Otoqi.
15.04.2020
Why influential women back Agnès Petit and her concrete robot
Agnès Petit, CEO and founder of Mobbot, wants to change the ways the construction industry works. This is, to put it mildly, quite a challenge. But Agnès has found powerful allies who help her along the way. In this interview, two of them, investor Sylvie Mutschler and architect Birgitta Schock, explain why.
19.08.2019
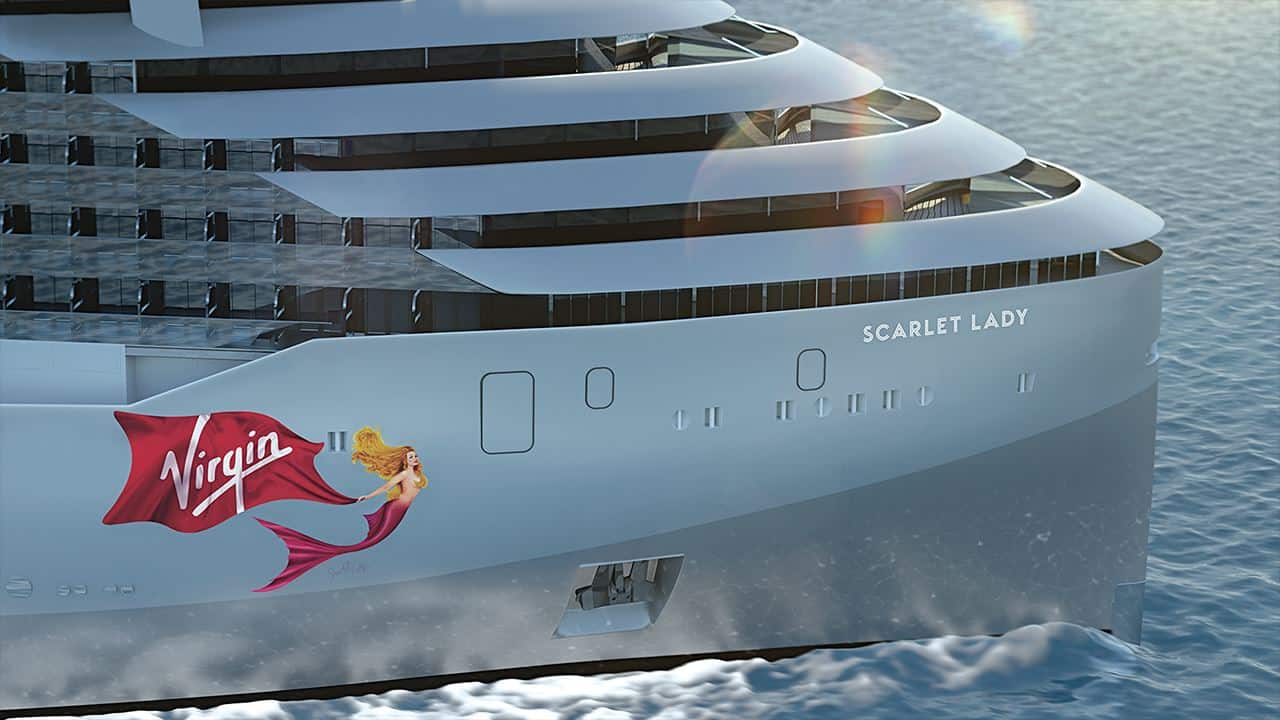
Why companies and families need a mission
Gabriel Baldinucci is a successful entrepreneur and was Vice President on the New Ventures team at Richard Branson’s Virgin Group. He’s now developing new projects for Singularity University in Santa Clara, California. In this interview, Gabriel talks about the importance of innovation for corporations and wealthy families.
Startups,Innovation andVenture Capital
Sign up to receive our weekly newsletter and learn about investing in technologies that are changing the world.